Cancer immunotherapy has reached a breakthrough in 2013 with the advent of drugs based on immune checkpoint blockade. However, even the most effective treatment options in immunotherapy result in an objective clinical response in only a minority of patients.
Impact of virally-derived components in anti-tumoral immune responses and lymphocyte migration
One approach for inducing antitumor immunity is to mimic the immune activation resulting from infectious agents by using synthetic ligands. Two receptor families of the innate immune system play a key role in the detection of microbial agents: the membrane-bound Toll-like receptors (TLRs) and the cytoplasmic RIG-I-like receptors (RLRs). The controlled pharmacological activation of these receptors to induce anticancer immune responses represents the major focus of our laboratory.
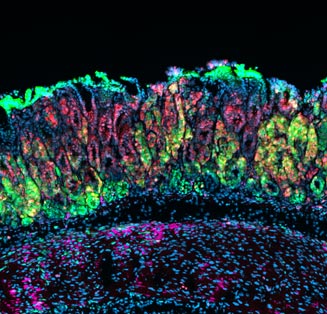
We are studying how the controlled activation of TLRs and RLRs can induce a stronger anti-tumoral immune response, following two main research lines. First, we are analyzing how specific drug combinations, administered with precise timings, influence the establishment of an anti-tumoral immune response by inducing a stronger T-cell and NK-cell anti-tumoral activity, and by inhibiting immune-suppressive mechanisms induced by the tumor itself. Secondly, we are studying how the activation of innate immune receptors impact on the migration of lymphocytes, with the final aim to enhance the recruitment of T-cells into tumors.
Design of tumor-targeted immunostimulatory nanoparticles (TiNaps)
Another major research focus of our lab is to develop and test new strategies for controlled drug delivery, based on the use of nanoparticles. Nanoparticles represent a potentially efficient drug carrier system, considering the multiple possibilities of design formulations with defined mechanisms of drug release and targeting.
We are currently testing different nanoparticle formulations for their safety and their efficacy in delivering the drugs to specific cell types of the immune system, such as antigen-presenting cells. The final aim is to develop tumor-targeted immunostimulatory nanoparticles (TiNaps) able to induce a more effective and targeted anti-tumoral immune response.
Tumor and immune cell metabolism: how do they interplay for the development of tumor-related immune responses
Tumor cells show an altered metabolism in order to support their high demand of energy required for cell proliferation, angiogenesis and metastasis formation. A potential method to treat tumors is to target their metabolic pathways, and block the energy support they need. In addition, tumor cell-derived metabolites can affect the development of an efficient anti-tumoral immune response, contributing for example in the creation of an immune-suppressive microenvironment. We are studying the function of specific components of tumor-related metabolic pathways, and how their blockade affects tumor cell proliferation and influences the tumor-related immune response.
A parallel research line is to undercover the metabolic features of anti-tumoral T lymphocytes, and to investigate approaches that target T-cell metabolism and could result in an improved anti-tumoral T-cell-mediated immune response.
This project is part of the Innovative Training Network Immutrain funded by the European Union’s Horizon 2020 research and innovation programme under the Marie Skłodowska-Curie grant agreement No 641549 - http://www.immutrain.eu/
